Stomach ulcers, also known as peptic ulcers, are open sores that develop on the lining of the stomach or the first part of the small intestine. These painful lesions can significantly impact an individual’s quality of life, causing discomfort and leading to more severe health issues if left untreated. Understanding the symptoms, causes, and treatment options for stomach ulcers is crucial for effective management and recovery. In this guide, we will explore the various aspects of stomach ulcer symptoms, providing clear and comprehensive information to help you navigate this common yet often misunderstood condition.
Symptoms of Stomach Ulcers
Recognizing the symptoms of stomach ulcers is vital for timely diagnosis and treatment. Common symptoms include:
Common Stomach Ulcer Symptoms
– Burning Stomach Pain: This is the most prevalent symptom, often felt in the upper abdomen. The pain may improve or worsen with eating.
– Bloating: A feeling of fullness or swelling can accompany the pain.
– Nausea and Vomiting: Many individuals with ulcers experience feelings of nausea, and some may vomit, which can sometimes include blood.
– Indigestion: Symptoms like heartburn and discomfort after meals can occur.
Rare Stomach Ulcer Symptoms
– Vomiting Blood: This is a serious symptom indicating bleeding in the stomach and requires immediate medical attention.
– Dark or Tarry Stools: This can indicate bleeding in the upper gastrointestinal tract.
– Unexpected Weight Loss: Unintentional weight loss can occur due to pain or discomfort leading to decreased appetite.
– Anemia: Continuous bleeding from an ulcer can lead to anemia, characterized by fatigue and weakness.
Understanding these symptoms can help individuals seek medical advice promptly, preventing complications.
Causes & Risk Factors
Several factors contribute to the development of stomach ulcer symptoms. Understanding these can help in prevention and management.
H. pylori Infection
Helicobacter pylori (H. pylori) is a type of bacteria that can infect the stomach lining. It is one of the primary causes of peptic ulcers, as it disrupts the protective mucous layer, allowing stomach acid to damage the lining. H. pylori infection is quite common worldwide, with a significant portion of the population being affected at some point in their lives. The bacteria are typically transmitted through contaminated food or water, or through direct contact with saliva or bodily fluids from an infected person.
Once H. pylori establishes itself in the stomach, it can lead to chronic inflammation known as gastritis, which may present symptoms such as abdominal pain, bloating, nausea, and indigestion. In some cases, the infection can lead to more severe complications, including peptic ulcers and an increased risk of gastric cancer.
Diagnosis of H. pylori infection can be performed through various methods, including breath tests, blood tests, stool tests, and endoscopy with biopsy.
NSAID Overuse
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and aspirin, can irritate the stomach lining when taken frequently or over prolonged periods. This increases the risk of ulcer formation. Additionally, NSAIDs can interfere with the normal production of protective mucus in the stomach, further exacerbating irritation and inflammation. This increased acidity and decreased mucosal defense can lead to symptoms such as heartburn, nausea, and abdominal pain. In some cases, chronic use of NSAIDs can result in gastrointestinal bleeding and perforation, which are serious complications that may require medical intervention.
To mitigate these risks, healthcare professionals often recommend taking NSAIDs with food or milk, which can help buffer the stomach lining. Alternating NSAIDs with other pain management strategies, such as acetaminophen, may also be advisable. For individuals with a history of ulcers or gastrointestinal issues, the use of protective medications, such as proton pump inhibitors or misoprostol, may be considered to help safeguard the stomach.
Stress
While stress itself does not directly cause ulcers, it can exacerbate symptoms and contribute to behaviors (like increased NSAID use or unhealthy eating) that may lead to ulcers. Additionally, stress can influence the body’s production of stomach acid and affect the overall balance of the digestive system. When under stress, individuals may experience changes in appetite, leading to overeating or skipping meals, both of which can disrupt normal digestive processes. Furthermore, stress might impair the body’s ability to heal existing ulcers by triggering inflammatory responses or by altering gut microbiota composition, potentially hindering recovery.
Smoking and Alcohol
Both smoking and excessive alcohol consumption can interfere with the stomach’s protective mechanisms, making individuals more susceptible to ulcers. Both smoking and excessive alcohol consumption can interfere with the stomach’s protective mechanisms, making individuals more susceptible to ulcers. Smoking impairs the production of bicarbonate, which neutralizes stomach acid, and can also decrease the effectiveness of the mucosal barrier that protects the stomach lining. Additionally, nicotine may increase gastric acid secretion, further exacerbating the risk of ulcer formation.
Excessive alcohol consumption, on the other hand, irritates the stomach lining and can lead to inflammation (gastritis), which compromises the protective barrier. Chronic alcohol use also disrupts the balance of gut bacteria, potentially leading to an overgrowth of harmful microorganisms that can damage the lining of the stomach.
Genetic Factors
A family history of ulcers may increase an individual’s risk, indicating a potential genetic predisposition to developing these conditions. Additionally, environmental factors such as diet, stress levels, and the use of nonsteroidal anti-inflammatory drugs (NSAIDs) can also play significant roles in ulcer development. Individuals with a family history of ulcers should be particularly mindful of these risk factors, as they may exacerbate any existing vulnerabilities.
Moreover, lifestyle choices, including smoking and excessive alcohol consumption, have been linked to a higher incidence of peptic ulcers. It is essential for those with a familial background of ulcers to engage in preventive measures, such as adopting a balanced diet rich in fruits and vegetables, managing stress through relaxation techniques, and avoiding irritants. Regular medical check-ups can also aid in early detection and management of any symptoms that may arise.
Diagnosis
Diagnosing stomach ulcer symptoms typically involves several medical tests to confirm the presence of ulcers and rule out other conditions.
Medical Tests
– Endoscopy: A procedure where a thin tube with a camera is inserted into the digestive tract, allowing the doctor to view the ulcer directly.
– Breath Test: This test checks for H. pylori by analyzing the patient’s breath after ingesting a specific solution.
– Blood Tests: These can help detect H. pylori infection and check for anemia.
– Stool Tests: Samples may be analyzed for the presence of H. pylori and signs of bleeding.
Importance of Diagnosis
Early diagnosis is crucial to prevent complications like bleeding or perforation of the ulcer, which can be life-threatening. Timely identification of ulcer symptoms enables healthcare providers to initiate appropriate treatment plans, such as lifestyle modifications, medications, or in severe cases, surgical intervention. Additionally, patients should be educated on the importance of recognizing early signs of ulcers, including persistent abdominal pain, bloating, nausea, and changes in appetite.
Regular check-ups and monitoring can play a significant role in managing risk factors associated with ulcers, such as the use of nonsteroidal anti-inflammatory drugs (NSAIDs), excessive alcohol consumption, and Helicobacter pylori infection.
Treatment Options
Treatment for stomach ulcers focuses on relieving symptoms, promoting healing, and preventing further complications.
Medications
– Proton Pump Inhibitors (PPIs): These medications reduce stomach acid production, allowing ulcers to heal. Common PPIs include omeprazole and lansoprazole.
– Antibiotics: If H. pylori is present, antibiotics are prescribed to eradicate the infection.
– Antacids: These can provide quick relief from ulcer pain by neutralizing stomach acid.
– H2-receptor antagonists: These medications also reduce acid production and can be used alongside PPIs.
Lifestyle Changes
– Dietary Adjustments: Eating smaller, more frequent meals can help manage symptoms. A diet rich in fruits, vegetables, and whole grains is recommended.
– Avoiding Triggers: Identifying and avoiding foods or substances that worsen symptoms (like spicy foods, caffeine, and alcohol) is essential.
– Stress Management: Techniques such as meditation, yoga, or counseling can help reduce stress levels.
Natural Remedies
Some individuals find relief through natural remedies, such as:
– Probiotics: These can help restore the balance of good bacteria in the gut and may aid in healing.
– Honey: Known for its antibacterial properties, honey may promote healing.
– Licorice Root: This herb may help protect the stomach lining.
Consultation with Healthcare Providers
Before starting any treatments or remedies, it’s crucial to consult with a healthcare provider to ensure safety and effectiveness. Before starting any treatments or remedies, it’s crucial to consult with a healthcare provider to ensure safety and effectiveness. They can provide personalized guidance based on your individual health status, medical history, and any medications you may already be taking. Self-diagnosing and self-treating can lead to unintended side effects or interactions, potentially worsening your condition rather than improving it.
Additionally, a healthcare provider can help determine the most appropriate course of action, whether that’s lifestyle changes, over-the-counter solutions, or prescription medications.
Complications & When to See a Doctor
Untreated stomach ulcer symptoms can lead to serious complications. Recognizing when to seek medical attention is vital.
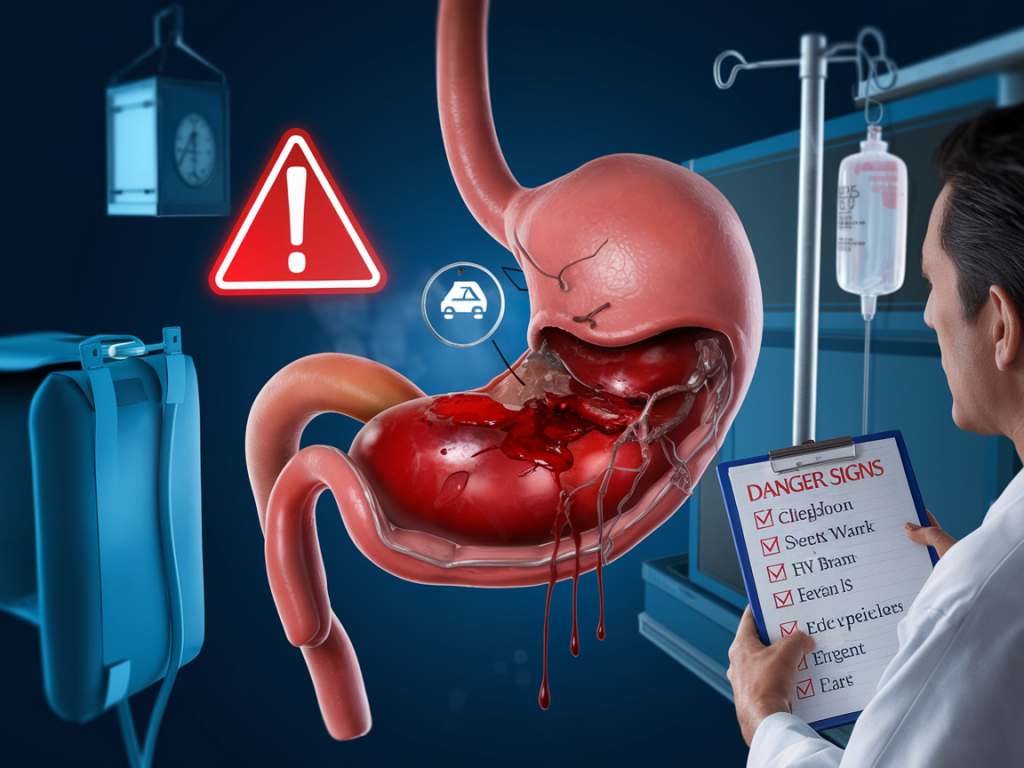
Complications
– Bleeding Ulcers: Ulcers can bleed, resulting in vomiting blood or having dark, tarry stools. This situation requires immediate medical intervention.
– Perforation: A severe complication where the ulcer creates a hole in the stomach wall, leading to peritonitis, a life-threatening condition.
– Obstruction: Swelling from ulcers can block the passage of food through the digestive tract, causing severe pain and vomiting.
When to Seek Medical Attention
– Persistent abdominal pain that worsens.
– Signs of bleeding (vomiting blood or passing dark stools).
– Severe nausea or inability to eat or drink.
– Unexplained weight loss or fatigue.
Prevention Tips
Preventing stomach ulcers involves adopting healthy lifestyle choices and managing risk factors.
Diet
– Balanced Diet: Eat a variety of foods, including fruits, vegetables, whole grains, and lean proteins.
– Avoid Triggers: Identify and limit foods that irritate your stomach.
Stress Management
– Mindfulness Practices: Incorporate relaxation techniques like meditation and deep breathing exercises.
– Adequate Sleep: Ensure a good night’s sleep to promote overall well-being.
Avoiding NSAIDs
– Talk to Your Doctor: If you require pain relief, discuss alternative medications that are less likely to irritate the stomach lining.
Smoking Cessation
– Quit Smoking: Seek support to quit smoking, as it significantly reduces ulcer risk.
Myths vs. Facts
Clearing up misconceptions about stomach ulcers can enhance understanding and awareness.
Myth: Spicy Foods Cause Ulcers
Fact: While spicy foods can irritate an existing ulcer, they do not cause ulcers. The primary causes include H. pylori infection and NSAID use.
Myth: Stress Causes Ulcers
Fact: Stress does not directly cause ulcers but can exacerbate symptoms and affect eating habits.
Myth: Ulcers Only Affect Older Adults
Fact: While more common in older adults, stomach ulcers can occur at any age, including in children and young adults.
Conclusion
Stomach ulcers are a common condition that can lead to serious health issues if not addressed. By understanding the symptoms, causes, and treatment options available, individuals can take proactive steps in managing their health. If you suspect you have a stomach ulcer or are experiencing any concerning symptoms, consult with a healthcare professional for a proper diagnosis and personalized treatment plan.
FAQ Section
Can stress cause ulcers?
Stress does not directly cause ulcers but can worsen symptoms and lead to unhealthy behaviors that contribute to ulcer formation.
How long does ulcer treatment take?
Treatment duration varies but typically lasts 4 to 8 weeks, depending on the severity of the ulcer and the prescribed treatment plan.
Are stomach ulcers contagious?
No, stomach ulcers are not contagious. They are primarily caused by H. pylori infection or NSAID use.
Can diet alone heal an ulcer?
While a healthy diet can support healing, it is essential to follow a comprehensive treatment plan including medications prescribed by a healthcare provider.
What foods should I avoid if I have an ulcer?
Avoid spicy foods, caffeine, alcohol, and any specific foods that trigger symptoms for you. Always consult with your healthcare provider for personalized advice.